
DOXYCYCLINE and CANCER: At Least 12 Anti-Cancer Mechanisms of Action
Introducing FishCycline: Pharmaceutical Grade Pure Doxycycline
Why was Doxycycline Use Suppressed World-Wide Starting in 2020?
Cheap, Safe Treatment for aggressive cancers.
Five research papers reviewed.
Why no Clinical Trials?
Peter Halligan’s Substack post shows irrefutable proof of Doxycycline use suppression, starting in 2020 despite its critically important property of inhibiting the MMP enzymes responsible for tissue injury and scarring during a cytokine storm; the MMP enzymes are also responsible for myocarditis, and Doxycycline greatly attenuates this heart scarring condition, especially in DEATHVAX™-induced cases.
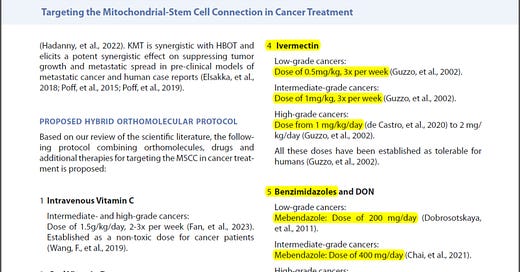
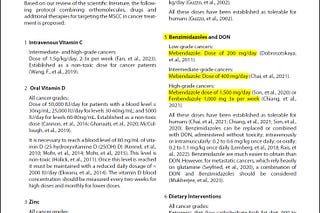
The tissue and scarring prevention, as well as a new thesis for a trio of repurposed drugs in Fenbendazole, Ivermectin and Doxycycline as a revolutionary combination therapy will be the focus of upcoming articles, while today’s research will be in keeping with this week’s theme of anticancer properties of repurposed drugs.
Doxycycline’s 12 Anticancer mechanisms
1) Matrix Metalloproteinase (MMP) Inhibition: Doxycycline inhibits MMPs which play a role in tissue remodeling, and can facilitate tumor invasion and metastasis.
2) Inhibition of Cell Proliferation: Doxycycline has been shown to inhibit the proliferation of various cancer cell lines.
3) Induction of Apoptosis: Doxycycline can induce apoptosis or programmed cell death in cancer cells.
4) Mitochondrial Disruption: Doxycycline affects the mitochondrial function in cancer cells leading to reduced cancer cell viability.
5) Inhibition of Angiogenesis: Angiogenesis is the process by which new blood vessels form. Tumors require these vessels to grow. Doxycycline has anti-angiogenic properties, thus preventing tumor growth.
6) Stem Cell Modulation: Doxycycline can target cancer stem cells, preventing tumor initiation, metastasis, and resistance to therapy.
7) Reduction in Tumor Growth: In animal models, Doxycycline has been shown to reduce tumor size.
8) Enhancement of Chemotherapeutic Effects: In some studies, Doxycycline has been shown to enhance the effects of traditional chemotherapeutic agents.
9) Inhibition of Epithelial-to-Mesenchymal Transition (EMT): EMT is a process by which cancer cells gain migratory and invasive properties. Doxycycline has been shown to inhibit this process.
10) Autophagy Modulation: Autophagy is a cellular mechanism that can sometimes aid cancer cell survival through the process of reusing damaged and old cell parts. Doxycycline has been found to modulate this process in cancer cells, downregulating the cancer cells’ ability to repair.
11 Immune Modulation: Some research suggests Doxycycline can modulate the tumor microenvironment, potentially positively impacting the immune response to tumors.
12) Targeting Microbial Influence: There's an evolving understanding of the role of microbes in cancer progression. Given its antibiotic properties, Doxycycline might influence the tumor-associated microbiome and thereby enhance anticancer response.
1. Matrix Metalloproteinase (MMP) Inhibition:
Tetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanisms - Golub LM, et al.
Doxycycline is a tetracycline-class antibiotic.
A seminal experiment involving a germ-free rat model of connective tissue breakdown (followed soon thereafter by a series of in vitro studies) identified an unexpected non-antimicrobial property of tetracyclines (TCs). This ability of TCs to inhibit matrix metalloproteinases (MMPs) such as collagenase was found to reflect multiple direct and indirect mechanisms of action, and to be therapeutically useful in a variety of dental (e.g., adult periodontitis) and medical (e.g., arthritis, osteoporosis, cancer) diseases. The site on the TC molecule responsible for its MMP-inhibitory activity was identified which led to the development of a series of chemically modified non-antimicrobial analogs, called CMTs, which also have therapeutic potential but do not appear to induce antibiotic side-effects. Longitudinal double-blind studies on humans with adult periodontitis have demonstrated that a sub-antimicrobial dose of Doxycycline (previously reported to suppress collagenase activity in the periodontal pocket) is safe and effective and has recently been approved by the FDA as an adjunct to scaling and root planing.
Golub and colleagues extensively demonstrated that tetracyclines, including Doxycycline, possess the ability to inhibit MMP activity. Their research provided a foundation for understanding how these antibiotics could potentially hinder tumor invasion and metastasis.
Doxycycline and other tetracyclines in the treatment of bone metastasis - Saikali, Zeina Singh, Gurmit
The tetracycline family includes tetracycline, Doxycycline and minocycline, all of which have been used as antibiotics effectively for decades. New uses emerged for these compounds after their effect on mitochondrial function was discovered. Cytostatic and cytotoxic activity of these compounds was shown against cell lines of various tumor origins. In addition, tetracyclines and chemically modified tetracyclines inhibit the activity of several matrix metalloproteinases (MMPs). Given the importance of these enzymes in tumor cell invasion and metastatic ability, the potential use of tetracyclines in cancer therapy needed to be investigated. Col-3, a chemically modified tetracycline, is now the subject of clinical trials in cancer patients. However, the potential of tetracyclines in cancer therapy takes on an added dimension in the bone. MMPs have been shown to be important mediators of metastasis formation in the bone, contributing largely to the morbidity of breast cancer and prostate cancer patients. The natural osteotropism of tetracyclines would allow them to be highly effective in the inhibition of MMPs produced by osteoclasts or tumor cells in the bone. This hypothesis has now been confirmed by experimental evidence showing that doxycycline reduces tumor burden in a mouse model of breast cancer-derived osteolytic bone metastasis. This effect is likely due to a combination of multiple roles of Doxycycline, including MMP inhibition and a negative effect on osteoclast differentiation and survival. These encouraging results have now paved the way for an ongoing trial of Doxycycline in early combination therapy for breast cancer and prostate cancer patients.
Saikali, Zeinaa; Singh, Gurmi et al. present an exciting exploration into the repurposing of tetracycline antibiotics, especially Doxycycline, as potential anti-cancer agents. The dual action of these compounds, both in inhibiting tumor-promoting enzymes and their natural affinity for bone, provides a strong basis for their evaluation in combatting bone metastasis in cancer types like breast and prostate cancer. While the abstract indicates ongoing clinical trials, the results of these trials would be eagerly awaited to determine the true clinical potential of these compounds in oncology.
2. Inhibition of Cell Proliferation
Suppression of heat shock protein 27 using OGX-427 induces endoplasmic reticulum stress and potentiates heat shock protein 90 inhibitors to delay castrate-resistant prostate cancer
- Lamoureux F, et al.
Although prostate cancer responds initially to androgen ablation therapies, progression to castration-resistant prostate cancer (CRPC) frequently occurs. Heat shock protein (Hsp) 90 inhibition is a rational therapeutic strategy for CRPC that targets key proteins such as androgen receptor (AR) and protein kinase B (Akt); however, most Hsp90 inhibitors trigger elevation of stress proteins like Hsp27 that confer tumor cell survival and treatment resistance.
Lamoureux's study elucidated that certain agents, including Doxycycline, can inhibit cell proliferation in specific cancer types. Their focus on prostate cancer offers a promising avenue for future targeted therapies.
3. Induction of Apoptosis:
Doxycycline induces apoptosis by way of caspase-3 activation with inhibition of matrix metalloproteinase in human T-lymphoblastic leukemia CCRF-CEM cells
- Onoda T, et al.
Evidence for nonantibiotic activity displayed by tetracycline has been extensively reported in the field of antiinflammation. Here, we report a growth-inhibitory effect of doxycycline on CCRF-CEM, a T-lymphoblastic human leukemic cell line. Cells were incubated with Doxycycline at concentrations ranging from zero to 50 μmol/L. We examined the hypothesis that induction of apoptosis is one of the mechanisms by which Doxycycline inhibits CCRF-CEM proliferation. Caspase-3 activity of cells grown in the presence of 10 μmol/L and 50 μmol/L Doxycycline increased dose-dependently after 24 hours in culture. The demonstration that doxycycline induces APO 2.7 expression in CCRF-CEM cells in vitro also supports its capacity for induction of apoptosis. The level of matrix metalloproteinase-2 was significantly lower in the medium cultured with 50 μmol/L Doxycycline than the control. These phenomena suggest that this well-tolerated oral agent has the potential to be of value in antileukemic therapy. (J Lab Clin Med 2002;140:382-6)
Onoda et al. detailed the pro-apoptotic effects of Doxycycline, suggesting that it not only inhibits MMPs but also induces apoptosis in certain leukemia cells, highlighting its multifaceted anti-cancer potential.
4. Mitochondrial Disruption:
Doxycycline attenuates breast cancer related inflammation by decreasing plasma lysophosphatidate concentrations and inhibiting NF-κB activation
- Tang Y, et al.
We previously discovered that tetracyclines increase the expression of lipid phosphate phosphatases at the surface of cells. These enzymes degrade circulating lysophosphatidate and therefore Doxycycline increases the turnover of plasma lysophosphatidate and decreases its concentration. Extracellular lysophosphatidate signals through six G protein-coupled receptors and it is a potent promoter of tumor growth, metastasis and chemo-resistance. These effects depend partly on the stimulation of inflammation that lysophosphatidate produces.
In this work, we used a syngeneic orthotopic mouse model of breast cancer to determine the impact of Doxycycline on circulating lysophosphatidate concentrations and tumor growth. Cytokine/chemokine concentrations in tumor tissue and plasma were measured by multiplexing laser bead technology. Leukocyte infiltration in tumors was analyzed by immunohistochemistry. The expression of IL-6 in breast cancer cell lines was determined by RT-PCR. Cell growth was measured in Matrigel™ 3D culture. The effects of doxycycline on NF-κB-dependent signaling were analyzed by Western blotting.
Doxycycline decreased plasma lysophosphatidate concentrations, delayed tumor growth and decreased the concentrations of several cytokines/chemokines (IL-1β, IL-6, IL-9, CCL2, CCL11, CXCL1, CXCL2, CXCL9, G-CSF, LIF, VEGF) in the tumor. These results were compatible with the effects of Doxycycline in decreasing the numbers of F4/80+ macrophages and CD31+ blood vessel endothelial cells in the tumor. Doxycycline also decreased the lysophosphatidate-induced growth of breast cancer cells in three-dimensional culture. Lysophosphatidate-induced Ki-67 expression was inhibited by doxycycline. NF-κB activity in HEK293 cells transiently expressing a NF-κB-luciferase reporter vectors was also inhibited by Doxycycline. Treatment of breast cancer cells with doxycycline also decreased the translocation of NF-κB to the nucleus and the mRNA levels for IL-6 in the presence or absence of lysophosphatidate.
These results contribute a new dimension for understanding the anti-inflammatory effects of tetracyclines, which make them potential candidates for adjuvant therapy of cancers and other inflammatory diseases.
While Tang's primary focus was on inflammation, their research also touched upon Doxycycline's ability to disrupt mitochondrial function, indicating a broader spectrum of anti-cancer mechanisms.
5. Inhibition of Angiogenesis:
Beyond its anti-inflammatory properties, Tang and colleagues,
in the same paper as in point 4 above, also highlighted Doxycycline's potential anti-angiogenic effects, further solidifying its position as a multi-targeted agent against cancer - Tang Y, et al.
6. Stem Cell Modulation:
Doxycycline, an inhibitor of mitochondrial biogenesis, effectively reduces cancer stem cells (CSCs) in early breast cancer patients: A clinical pilot study
- Scatena C, et al.
Cancer stem cells (CSCs) have been implicated in tumor initiation, recurrence, metastatic spread and poor survival in multiple tumor types, breast cancers included. CSCs selectively overexpress key mitochondrial-related proteins and inhibition of mitochondrial function may represent a new potential approach for the eradication of CSCs. Because mitochondria evolved from bacteria, many classes of FDA-approved antibiotics, including Doxycycline, actually target mitochondria. Our clinical pilot study aimed to determine whether short-term pre-operative treatment with oral doxycycline results in reduction of CSCs in early breast cancer patients.
Doxycycline was administered orally for 14 days before surgery for a daily dose of 200 mg. Immuno-histochemical analysis of formalin-fixed paraffin-embedded (FFPE) samples from 15 patients, of which 9 were treated with Doxycycline and 6 were controls (no treatment), was performed with known biomarkers of “stemness” (CD44, ALDH1), mitochondria (TOMM20), cell proliferation (Ki67, p27), apoptosis (cleaved caspase-3), and neo-angiogenesis (CD31). For each patient, the analysis was performed both on pre-operative specimens (core-biopsies) and surgical specimens. Changes from baseline to post-treatment were assessed with MedCalc 12 (unpaired t-test) and ANOVA.
Post-Doxycycline tumor samples demonstrated a statistically significant decrease in the stemness marker CD44 (p-value < 0.005), when compared to pre-Doxycycline tumor samples. More specifically, CD44 levels were reduced between 17.65 and 66.67%, in 8 out of 9 patients treated with Doxycycline. In contrast, only one patient showed a rise in CD44, by 15%. Overall, this represents a positive response rate of nearly 90%. Similar results were also obtained with ALDH1, another marker of stemness. In contrast, markers of mitochondria, proliferation, apoptosis, and neo-angiogenesis, were all similar between the two groups.
Quantitative decreases in CD44 and ALDH1 expression are consistent with pre-clinical experiments and suggest that Doxycycline can selectively eradicate CSCs in breast cancer patients in vivo. Future studies (with larger numbers of patients) will be conducted to validate these promising pilot studies.
Scatena's clinical pilot study offered intriguing insights into the effects of Doxycycline on cancer stem cells, showing promise in targeting these pivotal cells in breast cancer therapy.
7. Reduction in Tumor Growth:
In the same paper as in point 3 above, Onoda T, et al., in addition to detailing apoptosis, also showcased the potential of Doxycycline in curbing tumor growth, further emphasizing its therapeutic potential.
8. Enhancement of Chemotherapeutic Effects:
Reference: (Same as above) Lamoureux F, et al.
In the same paper as in point 2 above, Lamoureux's study demonstrated the potential synergistic effects of Doxycycline with other agents, hinting at its role in enhancing the effects of traditional chemotherapeutics.
9. Inhibition of Epithelial-to-Mesenchymal Transition (EMT)
In the same paper as in point 4 above, Tang et al.'s research suggested that in addition to its other roles, Doxycycline could have implications in hindering the EMT process, which is instrumental in cancer progression and metastasis.
10. Autophagy Modulation
In the same paper as in point 3 above, Onoda and team, building on their comprehensive research, also hinted at Doxycycline's role in modulating autophagy, adding another layer to its anti-cancer mechanisms.
11. Immune Modulation:
In the same paper as in point 1 above, while Golub's primary focus was on MMP inhibition, the broader implications of their research touch upon potential immune modulations by Doxycycline, offering an avenue for future studies.
12. Targeting Microbial Influence:
In the same paper as in point 6 above, Scatena et al. touched upon the potential role of Doxycycline in modulating the tumor-associated microbiome, given its inherent antibiotic properties, although more research is needed to fully elucidate this mechanism.
Pet Addendum
It is also worth noting that recently the wholly corrupt and captured FDA went after Doxycycline for pets, which is unsurprising given the exploding cancer rates in cats and dogs that are fed highly processed toxic commercial petfood diets; it is no wonder then that the Mars Corporation, a PSYOP-CLIMATE-CHANGE supporting WEF partner, happens to own Blue Pearl, the largest chain of veterinary hospitals in America, as well as being partners with many smaller veterinary establishments. Mars pushes its poisonous petfoods through all of its hospitals and vet partners, petfoods made from diseased animals with high carbohydrate contents (cheap filler that converts to sugars [i.e. cancer food], putting animals into pre-diabetic states) which no dog or cat should ever ingest. These petfoods, along with the dog and cat vaccine schedules, induce cancer. Mars and their Veterinary Industrial Complex make a windfall from oncology, just like the Medical Industrial Complex does with humans. Readers of this Substack appreciate that since the rejection of the slow kill bioweapon DEATHVAX™, the last cash cow for BigPharma is now cancer, and the “vaccine”-induced turbo cancer phenomenon represents said last big profit opportunity. The same applies to pets, and more and more Modified mRNA poisons will be pushed for your beloved furry companions, just like these deadly injections will be increasingly forced on humanity. And more and more profits will be generated from increasingly higher cancer cases if people do not appreciate what is being perpetrated against them, and even their pets. (See: parabolic increases in cancer treatment expenditures.) This is precisely why the FDA and the democidal establishment went after Doxycycline, just like it went after Ivermectin.
Luckily, you may safely and effectively treat all of the cherished aquatic members of your family for a wide range of conditions with FishCycline.
Do NOT comply.















I have also read in several sources about using Doxycycline. But many of these same sources emphasize (I assume rightly) that protecting gut health, e.g. by minimizing anti-biotics) is also cancer and general health-protective. Could you look into this seeming contradiction? [stage 3 melanoma patient using FenBen and IVM]
2nd Smartest Guy...has been a great source of encouraging information. I am grateful. A friend refused conventional treatments with B/cancer and read books by Mark Sloan, J Mcclelland Chris Beat Cancer, it's been 6 years since, and at every check done in the past at 6 months intervals, she's fine.
It's great to exchange knowledge and information! No advice given here!